If you've been following the updates from the Centers for Medicare & Medicaid Services (CMS) for remote physiologic monitoring (RPM), you know that 2021 is a big year. If you haven't been following these updates or are not sure what RPM is, you're still in a great place! There are many opportunities for pharmacists to collaborate with providers to offer this meaningful service to patients. Have you ever wanted to digitally collect blood pressure readings from patients, rather than having to rely on them to call you or bring in a piece of paper with historical readings? With RPM, you have the opportunity to have real-time access to this clinically relevant information to make more meaningful recommendations to your collaborating providers. Not only does RPM provide a way to supply a blood pressure device to a Medicare patient, it also gives them access to a clinical team that helps guide them through active management of their blood pressure. Even more, this service is not limited to blood pressure management! As long at is reasonable and necessary to monitor physiologic data for a patient's condition, CMS notes that these patients qualify for RPM services.
While there are many areas that CMS has clarified for RPM, the most memorable ones surround the question of eligible patients, number of days of readings required for billing, devices that qualify for RPM, and the requirement of "interactive communication." You can check out our previous blog post on the CMS proposals for 2021 to learn more about these details. Both new and established patients are eligible for RPM services during the public health emergency (PHE) but once this period ends, only established patients will be eligible for RPM services. CMS believes that patients who have established care with a provider will have a more meaningful RPM experience because the provider will have collected pertinent information needed to appropriately manage the patient's condition and develop a treatment plan. As far as the diagnosis codes that would qualify a patient for RPM, there is not a specific list of eligible diagnosis codes but as was noted above, it must be reasonable to monitor the physiologic parameter for the condition and RPM must guide the treatment plan for that condition.
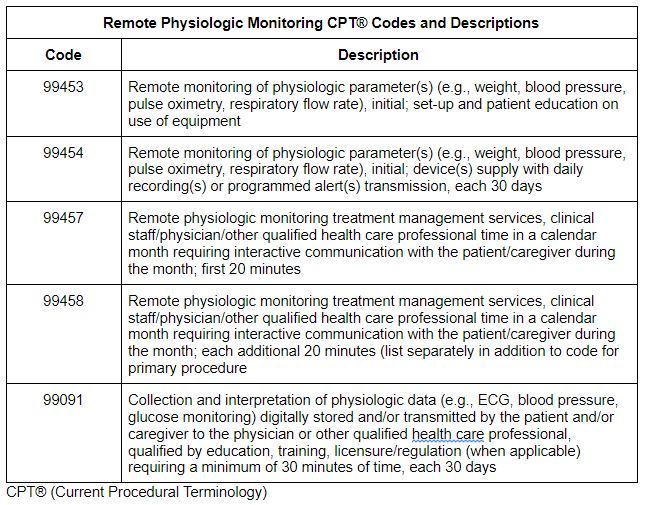
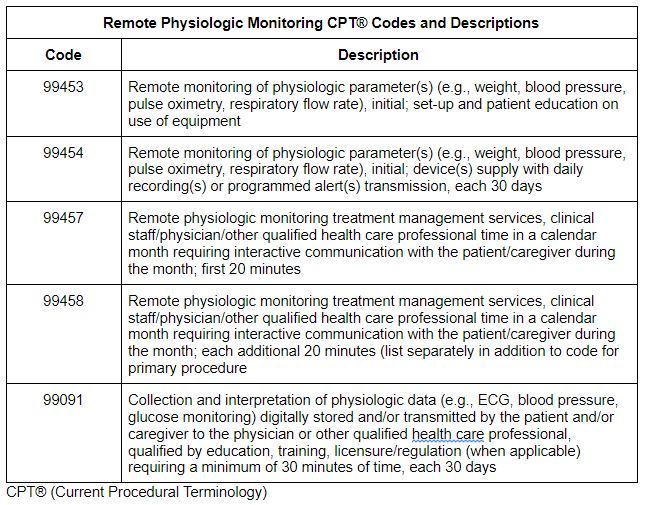
Similar to changes with new versus established changes, we will also see changes with the number of days of readings required to bill 99453 and 99454 once the PHE ends. During the PHE, it has been acceptable to bill 99453 and 99454 with a minimum of two days of readings but CMS will once again require a minimum of 16 days of readings after the PHE to bill these two codes. This makes sense as you need to have appropriate trends to make recommendations for the patient's treatment plan.
As was stated in the proposals for the final rule, the devices used for RPM services must meet the FDA definition of a medical device. Furthermore, the device must have the capability to digitally upload patient physiologic data, rather than relying on manual input of readings from the device to a platform. If manual patient entry were allowed, this would add room for human error in the process of obtaining readings. The selected device must be used to allow understanding of the current status of the patient. We have seen great value with RPM in our provider practices, identifying patients who are hypotensive and symptomatic, re-routing patients to care when follow-up is needed , and proactively managing disease states and providing education.
One of the final areas of clarification for 2021 was the requirement for "interactive communication" and what this means. If you look at the definitions for the RPM codes 99457 and 99458, you will see that there is a requirement for "interactive communication" with the patient or caregiver in order to bill for these codes. CMS clarified that this should be interpreted as a real-time interaction between the patient and the clinical staff member providing the service. Furthermore, this real-time communication must be at a minimum a two-way audio connection that is capable of being enhanced with other data transmissions, such as video connectivity. This means that texting or messaging services between the patient and clinical staff do not count towards "interactive communication" requirements.
The biggest discrepancy and area of confusion for our team was the difference between the published version of the final rule on December 28th and the CMS Fact Sheet released on December 1st. We had hoped that CMS would clarify how time is totaled during the calendar month for RPM services but this was not evident from the published version. The final rule stated that CMS believed that the "interactive communication" between a patient or caregiver and the clinical staff must total at least 20 minutes within the calendar month for 99457 to be billed. Furthermore, additional 20-minute increments of "interactive communication" would need to be accumulated within the calendar month for 99458 to be billed. This meant that the clinical staff team would be responsible for speaking to each patient enrolled in RPM for a minimum of 20 minutes each month and that time dedicated to monitoring readings, analyzing trends, and making clinical recommendations would not count towards the minimum time required for billing.
Fortunately, it was identified by CMS that the comments and responses surrounding codes 99457 and 99458 were unintentionally omitted from the published version of the final rule. A correction notice will be available from CMS in the near future that will confirm the statements from the CMS Fact Sheet that indeed both the time for care management services and the time for interactive communication with the patient and caregiver will count towards the time needed to bill 99457 and 99458. This is fantastic news for pharmacists who may be collaborating with providers as clinical staff and auxiliary personnel to assist in offering RPM services.
RPM is a valuable service for patients to have peace of mind knowing that the clinical team is actively monitoring their physiologic readings but it is also extremely valuable to pharmacists and providers who are managing patients with complex medication regimens and oftentimes multiple comorbidities. RPM provides the clinical team with more data to make informed decisions in the patient's care as we know that how patients present in the office is not always how they present at home. RPM is another clinical service that can be used to promote patient safety, optimal medication use, and improved clinical outcomes.
References:
2021 CMS PFS Final Rule