Remote patient monitoring involves the collection, assessment, and interpretation of digitally collected physiologic data. Patients are provided with devices to monitor readings in-between office visits. This provides the healthcare team with additional data to make more informed decisions in patient care. Oftentimes, we think of the patients with white coat hypertension and those who are at risk for falls due to hypotension when at-home monitoring is considered. Alternatively, we may consider at-home monitoring for patients who are high-risk and there may be concerns for medication non-adherence or worsening control of their disease states. RPM provides an opportunity to identify these patients proactively and adjust therapy as needed. Devices may include but are not limited to blood pressure monitors, scales, pulse oximeters, and glucometers.
Chronic Care Remote Physiologic Monitoring (RPM) Services, commonly referred to as remote patient monitoring or telemonitoring, are now allowable under general supervision as RPM has been designated as a care management service. This means that the supervising provider is not required to be in the same office suite as the individual performing or conducting the RPM service.1 This exciting news means that RPM services can now be offered in various locations, including the community pharmacy. Pharmacists who have established collaborative contracts with providers can now work as contracted employees or through other models to offer RPM to their patients.
As part of the final rule for 2020, CMS acknowledged the ambiguity surrounding the RPM program as they had not published strict guidelines for qualifications for RPM.1 Currently, RPM is a payable service for Medicare patients who would benefit from telemonitoring services. Copays and deductibles do apply for these services, so that must be taken into consideration when selecting an appropriate patient for enrollment.
The workflow of RPM may depend on the practice setting, but in the community pharmacy, this would involve collaborating with a supervising provider to identify patients who would benefit from the program. After patients are enrolled, they are provided with devices that connect to a clinician dashboard through various connection types. There are options for devices that connect cellularly as well as those that require a wireless network and Bluetooth connectivity. Additionally, there are patient wearables or devices that can be used regularly but do not require being connected to the patient at all times. Patients monitor their readings and the data is transmitted to the dashboard. The pharmacy team evaluates these readings on a regular basis and serves as triage to identify if further escalation is needed. Some readings can be addressed by a patient phone call while others may require more immediate attention by the provider or emergency services.
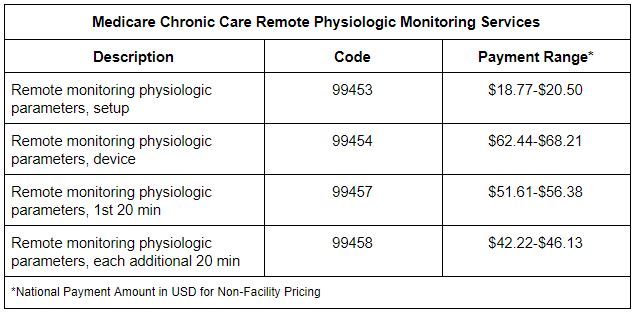
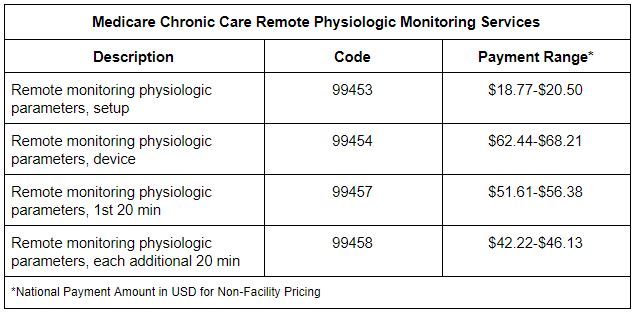
The Medicare program now includes four codes that can be billed by qualified healthcare professionals for the provision of RPM services. The initial code, 99453, is intended to cover the time and efforts dedicated to setting up the device for the member. This would include education on how to use the device as well as how to communicate with the team if there are any needs. The next code, 99454, is intended to cover the cost of the device and any costs associated with transmissions. This code is billable once every 30 days. Interestingly, this is the only RPM code that is based on a 30-day cycle, rather than a calendar month. Codes 99457 and 99458 are billable in increments of 20 minutes for clinical staff time dedicated to RPM services with 99457 attributed to the first 20 minutes and 99458 attributed to each additional increment of 20 minutes. These codes are billed based on time accumulated within the calendar month.
There are so many opportunities to make a positive impact on patient care. RPM has provided data to proactively identify patients who are non-compliant with medications. It has also served as a tool to connect uncontrolled patients with their providers for additional telehealth or in-office visits as needed. When a worsening trend is identified, the healthcare team reaches out to the patient to ask questions, provide recommendations, identify any needs that the patient may have, and connect them to resources. This provides patients with peace of mind, knowing that their healthcare team is working diligently to monitor their care.
References:
1. Centers for Medicare & Medicaid Services. Medicare Program; Revisions to Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B for CY 2019; Medicare Shared Savings Program Requirements; Quality Payment Program; Medicaid Promoting Interoperability Program; Quality Payment Program—Extreme and Uncontrollable Circumstance Policy for the 2019 MIPS Payment Year; Provisions From the Medicare Shared Savings Program— Accountable Care Organizations— Pathways to Success; and Expanding the Use of Telehealth Services for the Treatment of Opioid Use Disorder Under the Substance Use-Disorder Prevention That Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act. Woodlawn, MD: Federal Register, 2018.
2. Centers for Medicare & Medicaid Services. Physician Fee Schedule Look-Up Tool. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PFSlookup. Accessed July 14, 2020.